Dogs are exceptional at scent discrimination. Trained (and sometimes even untrained) dogs are capable of detecting numerous human diseases, such as cancer, by scent. Over the past 30 years, there have been several reports of dogs alerting their humans of a physical health issue.
1989: a patient’s dog persistently sniffed a mole on her leg, prompting the patient to visit a clinician, who identified the mole as a malignant melanoma1.
2001: a man’s dog persistently sniffed at a patch of eczema on his leg, which turned out to be a basal cell carcinoma2.
2013: a man’s dog persistently licked a lesion behind his right ear, which turned out to be malignant melanoma3.
More recently, Taverna et al. published a pivotal paper on the canine detection of prostate cancer— the second most prevalent cancer worldwide—from urine4. The dogs in this study detected prostate cancer with a mean sensitivity of 99% and mean specificity of 98%—supporting the notion that olfactory detection of prostate cancer holds is a promising path forward.

The problem
Prostate Specific Antigen (PSA) screening tests are used to detect prostate cancer, however they may miss clinically significant cancer in men with normal PSA levels and over-diagnose men with clinically insignificant cancer. We need more sensitive and specific non-invasive diagnostic technologies—particularly for differentiating between potentially lethal, high Gleason Grade cancers and low grade cancers that are less clinically severe. Using dogs trained to detect cancer by smell (canine olfaction), has been shown to be specific and sensitive. However dogs are impractical as scalable diagnostic strategies.
The solution
Guest et al. explore the idea of transforming canine olfaction into a machine olfaction system in the hopes of generating a scalable diagnostic solution in the future. The researchers explore what dogs may be detecting and if an artificial neural network (ANN) deployed in conjunction with machine olfaction can replicate the dogs’ early detection capability.
The approach and findings
The researchers tested the clinical feasibility of a multi-disciplinary, integrative approach to early prostate cancer biosensing in urine using trained canine olfaction, volatile organic compound (VOC) analysis, artificial neural network (ANN)-assisted examination, and microbial profiling in a double-blinded pilot study.
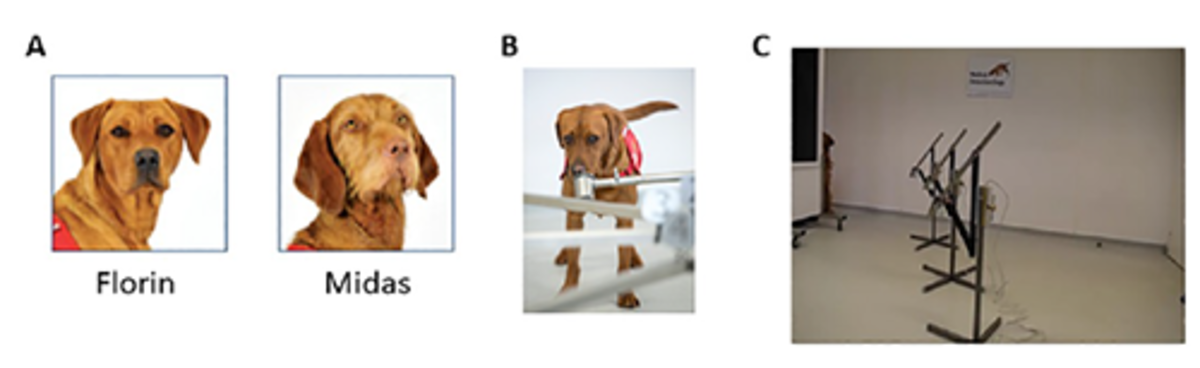
Two dogs were trained to detect Gleason 9 prostate cancer in urine collected from patients. The researchers used biopsy-negative controls to assess canine specificity in detecting prostate cancer.
The researchers collected urine samples from 12 patients with Gleason 9 prostate cancer and 38 biopsy-negative controls. The samples were analyzed for VOC content via gas chromatography-mass spectroscopy (GC-MS) and urinary microbiota content via 16S rDNA Illumina sequencing to identify key differentiators between cancer-positive and cancer-negative samples. The researchers used the dogs’ diagnoses to train an ANN to detect significant cancer-associated peaks in the GC-MS data.
Dog biodetection performance
The canine olfaction system was 71% sensitive and 70–76% specific at detecting Gleason 9 prostate cancer. Florin outperformed Midas in terms of specificity, but they were tied for sensitivity.
The researchers found that the training protocol impacted the dogs’ ability to correctly identify cancer-positive samples, but the dogs can adapt rapidly if appropriate reinforcement is given. You can learn more about the positive bias reward system (and other training methods) used in the study.
VOC and microbiota differences between cancer positive and biopsy-negative controls
Individual peaks representing VOCs were significantly elevated or reduced in prostate cancer versus biopsy-negative control urine samples. Specific to Gleason 9 prostate cancer samples, there were unique VOCs elevated compared with previous studies, including trimethyl silanol, a volatile siloxane resulting from silicone degradation.
The researchers did not see a clear difference in microbiota between cancer and healthy urine. However they did observe individual species of bacteria differentially abundant in cancer versus healthy urine. Dolosigranulum pigrum, a rare opportunistic pathogen, was elevated in Gleason 9 cancer samples.
An artificial neural network trained on canine olfaction diagnosis
The researchers used two techniques (skeletonization and auto-associative filtering) to identify critical chromatographic regions of VOC GC-MS data for informing canine diagnosis, and further identified peaks that were associated with cancer versus biopsy-negative control urines. Ultimately, they showed that an artificial neural network trained on canine olfaction is a feasible approach that should be pursued for prostate cancer diagnosis.
The impact
Guest et al. established a methodology to design larger-scale studies using canine olfaction, urinary VOCs, and urinary microbiota profiling to develop machine olfaction diagnostic tools. Eventually, scalable multidisciplinary tools should be tested against PSA screening to detect clinically aggressive prostate cancers earlier, non-invasively, and more specifically and sensitively.
References
- Williams H, Pembroke A. Sniffer dogs in the melanoma clinic? Lancet (London, England). 1989; 1 (8640):734. Epub 1989/04/01. https://doi.org/10.1016/s0140-6736(89)92257-5 PMID: 2564551.
- Church J, Williams H. Another sniffer dog for the clinic? The Lancet. 2001; 358(9285):930. https://doi.org/10.1016/S0140-6736(01)06065-2 PMID: 11575380
- Campbell LF, Farmery L, George SMC, Farrant PBJ. Canine olfactory detection of malignant melanoma. BMJ Case Reports. 2013; 2013:bcr2013008566. https://doi.org/10.1136/bcr-2013-008566 PMID: 24127369
- Taverna G, Tidu L, Grizzi F, Torri V, Mandressi A, Sardella P, et al. Olfactory system of highly trained dogs detects prostate cancer in urine samples. J Urol. 2015; 193(4):1382–7. Epub 2014/09/30. https://doi.org/10.1016/j.juro.2014.09.099 PMID: 25264338.